Baby health: symptoms you shouldn't ignore

Dr Anne Tait helps take the guesswork out of when to seek medical assistance, bringing parents one step closer to that all-important peace of mind.
Knowing when to take a child to the doctor can be a difficult decision. In the cooler months when there’s a lot of coughs and colds, snot and fevers around, the prospect of spending several hours waiting to be seen by an urgent doctor only to be told that it is a ‘viral illness’ can mean that such visits may be deferred. Nowadays there are a lot of sources of helpful information to guide parents, such as Health Line (0800 611 116), and of course, the ever-present Dr Google. However, the consequences of not seeking timely assessment can be scary, especially if a child is seriously unwell. This is particularly so when children get sick very quickly, despite initially appearing fine.
In this article I will review some common red flags – symptoms parents should look out for. This is not an exhaustive list but it focusses on the more common symptoms that children get. We should take care to note that some symptoms are more important in a certain age group but might not be that indicative of serious illness in other age groups. Clearly if a parent or caregiver is worried, then medical review should always be sought in the first instance. I always tell parents that I would much rather see mildly unwell children and provide reassurance, rather than see seriously unwell children who I think should have been reviewed earlier. Although clearly hindsight always has 20/20 vision.
FEVERS
Children commonly get fevers. This is an important part of the body’s immune response to illness. There is no correlation with the height of the fever and the severity of the illness. Certain viral conditions (ie influenza) can result in very high fevers. The general definition of a fever is anything higher than 38°C, although some sources state between 37.5°C and 38.3°C. All children will get fevers at some point in their childhood. Most of these are due to simple viral illnesses. However, fevers in young babies (under three months of age) are of particular concern. Children with fevers in this age group always need to be reviewed by a doctor, as due to their immature immune system, serious bacterial infection may be present. Children aged between three to twelve months of age with a fever should also be reviewed by a medical professional, but the urgency would be dependent on the presence of other symptoms. As a child gets older, need for medical review would be more dictated by whether they had any other symptoms of note, and also parental concern.
As children get older, the risk of serious infection in association with a fever becomes less, although it’s never zero – even in adults. If an older child is otherwise relatively well in themselves (ie alert, drinking, no other symptoms of note), then most fevers can be treated at home with simple strategies such as paracetamol, fluids and observation.
Prolonged fevers of more than five days’ duration should be reviewed by a medical professional as other causes (besides infection) may be present. This is especially so if fevers are more than seven days’ duration.

One of the complications of febrile illnesses can be a febrile convulsion. This is a relatively common issue in children between one to five years of age. It occurs in approximately one out of twenty children. It used to be thought that it was the height of the fever that caused the convulsion. However it is probably more the rapid spike in fever and/or certain viruses themselves. Unfortunately, regular use of antipyretics, such as paracetamol or ibuprofen, do not prevent febrile convulsions.
LETHARGY
We all feel lethargic and not ourselves when we are unwell. Lethargy itself is generally not a symptom to trigger warning, however if a child is lethargic to the point of not being easily roused or they’re unable to drink normally, then they should definitely be reviewed by a doctor.
VOMITING AND/OR DIARRHOEA
Gastroenteritis illnesses are one of the rites of passage of childhood. Fortunately, these are becoming less common with the implementation of the rotavirus vaccination and people being much more aware about hand hygiene. Vomiting and diarrhoea can be significant symptoms in very young children as they can easily lose large amounts of fluid and become dehydrated quickly. Certainly, children under one year of age with vomiting and diarrhoea should be seen by a medical professional. Older children should be reviewed if there are concerns about their hydration status and/or they are not able to keep any fluids down. Hydration can be assessed by looking at a child’s lips and tongue. If these are dry then a child does have mild dehydration. If their peripheries are cool, they are lethargic, and are not producing any tears, then prompt medical review is required, as these children are more significantly dehydrated.
Bilious vomiting (green bile) is one of those symptoms that always requires medical review. If children have profuse vomiting then they may have a small amount of blood in the vomit from a small tear in the lower oesophagus. This usually prompts very quick visits to the urgent doctor but usually does not require any intervention as the small tear will self resolve.
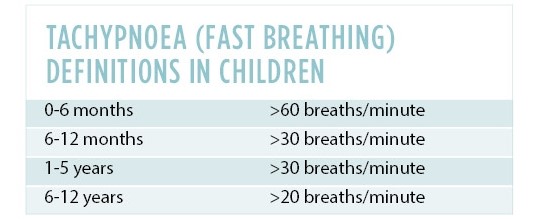
BREATHING DIFFICULTIES
Respiratory tract infections are another common ailment for all children but particularly those under the age of five years old. Common symptoms include coryza (snot), cough, increased respiratory rate, wheezing and increased work of breathing. Children under the age of one should be reviewed by a medical professional if they are having breathing difficulties. Again, this is because they can get very sick quickly at this age and they also may have low oxygen saturations that might not be recognised. Additionally, young children have great trouble feeding when they have a respiratory illness, which can cause them to get dehydrated reasonably quickly. Babies under six months breathe through their nose. If they are unwell with a respiratory tract infection, breathing always trumps feeding in their order of priority.
Breathing difficulties can be due to illness in any part of the respiratory tract. One of the important signs to look for is increased work of breathing. This relates to a child’s use of additional muscles to assist breathing. These include the intercostal muscles, chest wall, tracheal notch, head bobbing etc. If a child is needing to use additional muscles to aid breathing, then they definitely need medical review.
CRYING
Crying is one of those symptoms that babies and young children use to communicate their distress. All parents know that their children have many different cries which they can interpret. It’s hard to tell parents when to seek medical advice based on a cry, but I think it is generally one of those ‘gut feeling’ responses parents have to certain types of crying that are not the normal cries of hunger, annoyance, dirty nappy etc.
COMBINATION OF SYMPTOMS
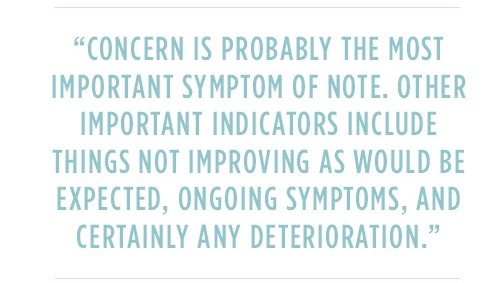
Most children generally have a combination of various symptoms when they are unwell. Examples of this include fever, vomiting and diarrhoea in the context of a gastroenteritis illness. Pneumonia typically presents with fevers, cough, fast breathing and increased work of breathing. Often when children are unwell, they tend to go off their solid food, and to a lesser extent, liquids.
Certainly, medical review should always be sought if a parent is concerned. Concern is probably the most important symptom of note. Other important indicators include things not improving as would be expected, ongoing symptoms, and certainly any deterioration. I always tell my patients that my advice at a review is a “snapshot at this particular point in time”, and certainly if things change, get worse or don’t improve within the expected time frame, then a repeat review is required. If a parent has ongoing concerns, then a second opinion (ie a fresh pair of eyes) can also be helpful.
|
Dr Anne Tait is a general paediatrician at Starship Children’s Hospital and Auckland Medical Specialists. She has an interest in all areas of children’s health and wellbeing. |

AS FEATURED IN ISSUE 43 OF OHbaby! MAGAZINE. CHECK OUT OTHER ARTICLES IN THIS ISSUE BELOW