Contraception after baby

Apart from the occasional harassed new father of four who has rushed straight from the hospital to organise a vasectomy for himself, new parents are often just too busy to give contraception much thought. Many couples assume that the mini-pill or condoms are their only option in the months after their baby is born but it is important to realise that there are many options, all of which have advantages and disadvantages. In all the excitement of having a new baby one important issue that often gets overlooked is how to avoid having another one. Dr Martin Sowter looks at the range of contraceptive options.
⚜️ When should I start?
The time it takes for fertility to return after having a baby varies greatly. Women occasionally will start ovulating again as early as four weeks after delivery so if you are not breastfeeding you should be using contraception from three weeks post-delivery if having intercourse.
⚜️ What method should I use?
Think through what you want from your contraceptive choice: convenience, reliability, no side effects, a quick return to fertility once stopped, or permanence. You are likely to be considering one of the options below:
⚜️ Lactational Amenorrhoea Method (LAM): The most convenient and side effect-free form of postnatal contraception is breastfeeding, or the Lactational Amenorrhoea Method, to give it its correct medical name. For most of the world's women this is the only option available to them. In New Zealand it's often not considered but it is a perfectly reasonable choice as long as you consider reliability and factors that increase its failure rate. Failure rates of only 2% have been reported, confirming it as an effective contraceptive choice. But this is with the proviso that women are not having any periods (this is called amenorrhoea), are exclusively breastfeeding every four hours and are not supplementing with any formula or expressed milk. Gaps of more than seven hours between any feeds reduce its reliability significantly and breast pumps appear less efficient at stimulating the production of hormones that stop ovulation. LAM also becomes much less reliable after six months of breastfeeding. And as ovulation can occur before a first period, the absence of periods at that time doesn't always mean it is still working. So, while LAM is a very reasonable option, many women would prefer to use additional methods in those first few months. All women should consider other options after six months.
⚜️ Natural family planning: Some women rely on natural family planning before having a baby, keeping a calendar of their menstrual cycle, monitoring cervical mucus and possibly supplementing that with kits that help determine the safest time to have sex. This method is much less reliable after you have had your baby and is difficult to use following on from LAM. In the first few months lochia, hormonal changes associated with breastfeeding and irregular ovulation makes monitoring cervical mucus difficult. There will also be a few months when LAM is no longer reliable but regular ovulation has not yet established. If you are using LAM and hoping to move onto natural family planning you should consider using condoms or other barrier method during this transition.
⚜️ Condoms and diaphragms: For child spacing, condoms are possibly the most widely used form of contraception. Easy to use and free of any hormonal side effects, they have a low failure rate of about 2% per year of use. Of course, they are ineffective if they stay in the drawer next to the bed and more than a few couples eventually get fed up with them, increasing the chances of an unexpected pregnancy. They are available on prescription after you have had a baby and although you're not going to get ones that glow in the dark or come with added warming lube, prescription condoms are as reliable as any you might buy yourself.
The diaphragm is in danger of disappearing as an option in New Zealand with only a few family planning clinics still able to offer them. This seems a real shame as it's easy to use and like condoms has no hormonal side effects. If combined with a spermicide the failure rate is comparable to condoms. All diaphragms look similar in appearance, consisting of a flexible latex cap with a firmer but bendy edge that sits over the cervix high in the vagina. They shouldn't be at all uncomfortable and can be inserted in the vagina a few hours before sex and taken out the next morning. Many contraceptive guides still discuss multiple types of diaphragm and caps, though in New Zealand you're likely to be offered only one choice.
If you plan on using the diaphragm for the first time fitting should be delayed until six weeks after delivery when the cervix is no longer dilated. If you used the diaphragm before your pregnancy then you will need to be refitted as both the vaginal tone and size of your cervix and vagina will have changed.
⚜️ The Intra-Uterine Contraceptive Device: Also called a coil, the IUCD is a T-shaped piece of plastic about 3cm long that is inserted through the cervix. A thin piece of nylon thread protrudes out through the cervix so it can be removed but it shouldn't be felt during intercourse. It can be inserted on the same day as baby is born but this is very rarely done in New Zealand, with most women having their IUCD fitted four to six weeks after delivery. There is a small risk of infection associated with insertion and some women complain of heavier or more painful periods when using an IUCD. Many women like the fact that it lasts at least five years and also has a very low failure rate, making it a very reliable choice.
⚜️ Mirena: This is very similar in appearance to an intra-uterine device but contains a reservoir of progestogen hormone that is slowly released over the next five years. Mirena is becoming an increasingly popular contraceptive choice for two reasons - it has a very low failure rate and most women will have much lighter or no periods. A Mirena can usually be inserted without anaesthetic and shouldn't be much more uncomfortable that having a cervical smear. You may experience irregular bleeding or spotting for the first month or two after insertion. Some women will have pre-menstrual symptoms from the progestogen but it usually settles over a few weeks.
It is a very safe form of contraception although some women experience ongoing irregular bleeding that ultimately means that Mirena isn't for them. The failure rate is similar to, or less than, female sterilisation so it's a good choice for a woman who thinks her family is complete but is not absolutely sure. It's also an excellent choice for women with heavy or painful periods or pain from endometriosis. One problem with Mirena is that it is relatively expensive, costing between $300 and $500, although over its life of fve years, you would save much more than that in sanitary products and doctor visits. Some clinics and hospitals can offer Mirena at no charge, particularly if it is used to treat heavy periods.
⚜️ Combined oral contraceptive pill: The "pill" contains two hormones - an oestrogen and a progestogen. Used properly it has a failure rate of well under 1% per year and continues to be one of the most popular contraceptive choices for women who are no longer breastfeeding. For women who are breastfeeding the combined pill isn't an option because it may interfere with breast milk production. The evidence that it has such an effect isn't actually very good but most doctors would advise against the combined pill at least until weaning has begun.
There is also some concern that oestrogens used after delivery might increase the risk of blood clots forming in the veins of the leg or lung. This is one of the rarer but most serious complications of the combined oral contraceptive. This risk falls quickly after delivery and women who are not breastfeeding could start the combined oral contraceptive pill as early as one month after the birth. One benefit of the combined pill is that periods will tend to be lighter and fertility usually returns quickly once it is stopped.
⚜️ The progestogen-only pill: Sometimes called the mini-pill, the progestogen-only pill doesn't contain oestrogen. It has a slightly higher failure rate compared with the combined pill of about 2% per year and does need to be taken at about the same time every day to minimise the risk of failure. It doesn't affect milk production and is generally regarded as very safe to use while breastfeeding. As with all progestogen-only contraception, a few women will have weight gain or mood changes but this is uncommon. Fertility returns as soon as it is stopped, making it an ideal choice for child spacing, but perhaps less than ideal if you need a very low failure rate.
⚜️ Contraceptive implants: Contraceptive implants consist of a series of small flexible plastic rods being inserted just below the skin in the arm where they release a low, continuous dose of progestogen. They are a very safe form of contraception with a failure rate comparable to sterilisation but some women will have irregular vaginal bleeding. Troublesome or inconvenient bleeding is the most common reason for being removed. Many women actually have much lighter or no bleeding. They are removed using a local anaesthetic and making a small incision over one end of the rods under your skin. The commonest implant used in New Zealand is called Jadelle and it consists of two rods about 4cm long and 3mm thick. There is a small risk of a local skin infection when the rods are inserted and occasionally they can be difficult to remove. One attraction is that they last up to five years and fertility returns very quickly once they are removed. Progestogen side effects similar to the mini-pill can occur.
⚜️ Depot Provera: This is a progestogen injection given every 12 weeks. It has a very low failure rate and many women have much lighter or no periods while using it. One potential disadvantage is that your fertility may take several months to return after your last injection and as with the implants, the mini-pill and Mirena, irregular bleeding can be a problem. After stopping, your bleeding pattern may also take longer to return to normal compared with other progestogen-only methods.
⚜️ Sterilisation: For couples not planning to have any more children, sterilisation is an option. However, don't let anyone persuade you that sterilisation is reversible. Both male and female sterilisation can be reversed but success rates are far from 100%, so you need to be certain that you want permanent and irreversible contraception.
Male sterilisation, or vasectomy, can be done using local anaesthesia and takes only about 20 minutes. A small cut is made over the vas deferens (the tube carrying sperm from the testicle) and this tube is then cut and its ends tied. It can take up to three months before no sperm is present in an ejaculate so you will still need to use other contraception until at least two samples are negative.
Female sterilisation is usually done through a laparoscope which is a long thin instrument with a camera attached that is inserted through an incision in the umbilicus (belly button) under a general anaesthetic. Another incision is made lower down and a small clip (about 1cm across) is put across the narrowest part of each fallopian tube blocking the passage of egg and sperm. Occasionally, female sterilisation needs to be done using a larger lower abdominal incision if the fallopian tubes can't be clearly seen.
Female sterilisation can also be done at the same time as a Caesarean section and makes no difference to the time taken to recover from surgery. You do need to be completely sure about your decision if you request a sterilisation or "tube tie" in this situation. There is a significantly higher proportion of women who regret their decision to be sterilised if it is done at the time of a C-section, compared with women who delay the decision.
When deciding between male and female sterilisation it is worth considering that vasectomy has the lowest failure rate of any form of contraception with only two to three failures per 1000 vasectomies, compared with five per 1000 for female sterilisation. A vasectomy is also safer than female sterilisation and a reversal can be attempted without the need for a difficult abdominal operation.
Reversing both a vasectomy and female sterilisation needs skilled micro-surgery with about 80% of couples having a baby after reversal. After a vasectomy reversal sperm may sometimes be present in an ejaculated sample but be of poor quality. Women having a sterilisation reversal are significantly more likely to have an ectopic pregnancy (a pregnancy in the fallopian tube). If reversal is unsuccessful IVF offers the only hope of having another baby.
Two newer methods of female sterilisation have recently been developed that use a hysteroscope. This is a very thin device with a camera attached that is passed through the cervix and a small plug or metal spring is placed inside the fallopian tube where it enters the uterus. Two techniques are available in New Zealand: Essure and Adiana. Both are simple day case procedures performed under local anaesthesia. They're available in only a few New Zealand hospitals but as they are both significantly safer than sterilisation performed through a laparoscope they are likely to become more popular. The main disadvantage of these new less invasive techniques is that they are completely irreversible and pregnancy is only possible after an Essure or Adiana procedure through IVF.
⚜️ Back in the swing ⚜️
Finally, of course, one question most couples ask is when they can start having sex again. The simple answer is probably when they feel ready. As long as no infection has occurred, stitches and tears should heal over a few weeks. Many women want to wait to resume having sex until they have had a postnatal examination four to six weeks after delivery. Women are sometimes surprised how much of a problem vaginal dryness is. This is a result of the change in hormone levels that occur with breastfeeding. It can be just as much of a problem in women who have had a C-section as women who have delivered vaginally. Lubrication can help but do talk to your doctor about using an oestrogen cream. This is safe to use while breastfeeding and can make a dramatic difference to discomfort during intercourse in the months after delivery.
Related articles
Lets talk about sex baby
Sex therapist tips: how to regain your mojo
5 Top Tips for Lasting Love
Keeping the spark alive
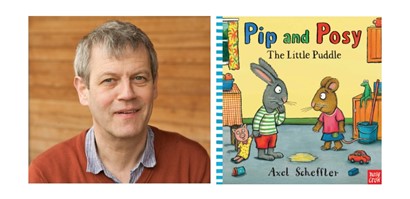
Martin Sowter (BSc MB ChB MD FRCOG FRANZCOG) is a part-time specialist at Auckland City Hospital in the fertility and menstrual disorders clinics. He also works privately as part of the specialist team at The Auckland Obstetric Centre. Over the past six years he has also been a regular visitor to the Cook Islands under the auspices of NZAID helping the local specialists with gynaecological surgery. Martin is married to Alison, an eye surgeon, and has two daughters.

AS FEATURED IN ISSUE 15 OF OHbaby! MAGAZINE. CHECK OUT OTHER ARTICLES IN THIS ISSUE BELOW