When pregnancy is a pain

Carrying another human being inside you puts extra strain on your body. Renée Vincent shares her tips on what you can do to ease those growing pains.
Magazines and social media overflow with images of glowing women floating blissfully through pregnancy. The reality for most is a little less glamorous and a lot more uncomfortable. Our bodies go through some wonderful changes to accommodate the little human growing inside. Unfortunately, some of those changes can lead to painful and, occasionally, debilitating conditions.
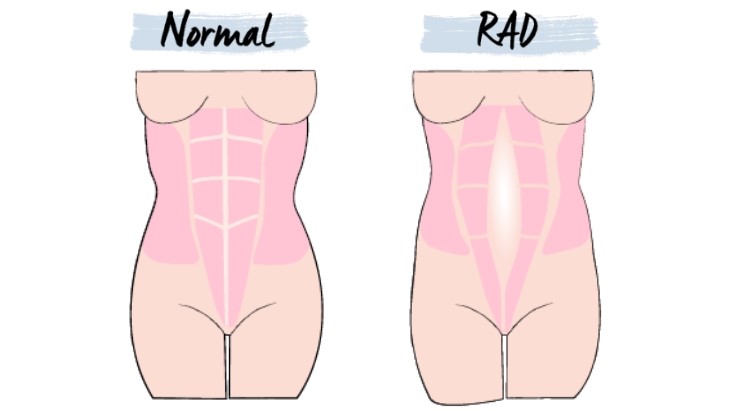
In the clinic I see women with a range of musculoskeletal problems, such as pelvic joint and lower back pain, rib and upper back pain, carpal tunnel syndrome or wrist pain, and abdominal muscle separation. These women are often scared and surprised because they don’t understand what’s going on. Luckily these conditions can be managed, and once you have the right information and know you’re not alone, you’ll be in a much better position to cope.
WHY IS PREGNANCY SO PAINFUL?
The musculoskeletal system sounds complicated but it’s just the bones, muscles, tendons and ligaments that hold us up and allow us to move. During pregnancy, changing hormones affect the body’s connective tissue and play a role in the aches and pains that occur. Levels of the relaxin hormone peak in the third trimester, but that isn’t the sole culprit; the increases in progesterone and oestrogen early in pregnancy also have an effect.
Some sources maintain these problems are due to an increase in ligament laxity, but the research findings are inconclusive. There are many things at play; it could be due to an increased vulnerability to the ligament tissue becoming painful or inflamed, combined with changes in posture and your shifting centre of gravity as the baby grows. This affects how your body balances and the load different structures are under. Fluid retention also influences the soft tissues and can cause painful nerve compression. Often we focus on the foetus, but forget that a woman’s whole body is also changing.
PELVIC PAIN
Pelvic girdle pain is the term given to pain occurring in the joints that connect the pelvis. You might feel this as pain at the top of your buttocks, in your tailbone, or in the pelvic connection at the front. Pain can also occur in your hips or thighs and is sometimes felt in the lower abdomen. Sometimes you also feel clicking or grinding in your pelvis area.
Pelvic girdle pain is very common and affects about 20% of pregnant women to some degree, at some time during pregnancy. Many women will only experience it for a few weeks, but around 6% will experience it severely or for several months. You’ll often feel the pain when you change positions in bed, stand up or sit down, climb stairs, or walk long distances.
Pain management tips: Always tell your Lead Maternity Carer (LMC) or obstetrician if you’re experiencing this kind of pain severely. If the pain is mild, you may be able to manage it yourself. It’s important to change positions regularly. When sitting, sit well back in the chair with your back against the back support, and, if possible, tilt the base of the chair down or sit on a pillow so that your knees are below your hips. When standing, try to stand on both feet evenly and shift your weight regularly. Draw yourself up tall and slightly tuck in your tail bone, supporting your bump with your abdominals by drawing them in slightly at your belt line.
If your pain is helped by rest, then try to have short rests, sitting or lying on your side, when you can. You need a balance between activity and rest – not too much of either. However, if you’re generally very active and busy, do your body a favour and slow down. Pace yourself by doing a little bit at a time and not too much in one day, which could make you too sore to do anything the next day.
When lying down on your side, you can try either a pillow between your legs, or the recovery position with one or two pillows under the knee that’s bent up. You may also find that a small pillow under your bump helps, or you can tuck a pillow behind your back. Experiment until you find what’s best for you.
It’s also helpful to modify your exercise and movement so that the pelvis is not being stretched or strained in an uneven position. You can modify your yoga routine, for example, by not sitting on the floor cross-legged or with your legs tucked to the side. Pregnancy support belts can also be very helpful for supporting the pelvis during weight-bearing activities like walking or doing work around the house. Swimming can be soothing and is less aggravating for many women.
If your pain is moderate-to-severe (you’d rate it more than four out of 10, with 10 being the worst), then you might like to see a physio, osteopath or chiropractor who specialises in pregnancy pain. They’ll use techniques, such as manipulation, massage, acupuncture, exercises and heat or cold therapy, to help relieve the pain and give you personalised advice and support. If your pain is severe and doesn’t respond to treatment, there are some medications you can take that make a difference, so don’t despair!
|
ABDOMINAL MUSCLE SEPARATION Pain management tips: Wearing a belly support can help reduce the strain on your abdominal muscle. These can be fitted by a women’s health physio. In addition, engaging your abdominals when standing, lifting or changing position can help support the RAD. Avoid heavy lifting or straining during exercise, and don’t overwork your abdominals in awkward positions. And take care to roll over before sitting up. Once baby is born, get your LMC to check your RAD (helpful for all postnatal women) before they discharge you, and to refer you to a physio if you still have a gap larger than 2cm. If you have trouble sitting up from lying on your back, or have pain and haven’t had your RAD checked, then it’s worth a visit to your GP or a women’s health physio.
|
UPPER BACK AND RIB PAIN
Although not as common as pelvic girdle pain, upper back or rib pain can cause considerable discomfort during pregnancy. Your upper back is affected by your posture changes caused by the baby bump, and also has to balance the increasing weight of your breasts. The ribcage and upper back work together, and the rib cage changes shape during pregnancy, widening through the base to allow room for the foetus. Often women will go up a bra size due to this increase in chest circumference – this change can be permanent if your ribs remain flared after pregnancy. These changes can result in the joints and muscles of the upper back and/or between the ribs and cartilage becoming very painful.
Pain management tips: If this is you, choose a good supportive maternity bra with wide straps for maximum support. It can be worth getting fitted professionally. Good posture when sitting is really important. If you work in an office, this could mean a completely different chair, cushions to give extra back support, or even sitting on a Swiss ball. When standing, draw yourself up tall and engage your abdominals gently to support your bump. Avoid or modify activities where you have to spend long periods twisted to one side or hunched forward with rounded shoulders.
It helps to take regular breaks from sustained activities and to do gentle stretches, such as reaching up and over with your arms to open the ribcage, or stretching your arms behind you, hands clasped, to open up the chest and move the upper back. If the pain is constant and not settling, or is severe, talk to your LMC or GP and see a physio to help restore normal movement and advise on what might be aggravating the pain.
SORE WRISTS
Carpal tunnel syndrome is surprisingly common during pregnancy, especially in the third trimester. You might notice pain or numbness in your wrists, as well as pins and needles and weakness in your fingers and hands. The pain may radiate up into your forearms. This problem is caused by compression of the wrist’s median nerve where it runs through the carpal tunnel. It’s more common in the third trimester because it’s related to fluid retention and swelling, which causes nerve compression. The symptoms will often be worse at night or when you’re doing repetitive work with your hands or leaning on your wrists. Most symptoms will resolve fully when your baby is born; and any residual symptoms usually resolve themselves within a few weeks.
Pain management tips: You can get substantial relief by wearing a wrist brace at night to keep your wrist in a neutral position. It’s also important to avoid or modify activities that aggravate your wrist as much as possible. See a physio or hand therapist, who can use massage, therapeutic ultrasound, gentle nerve exercises and give advice to help you manage the symptoms. They can also refer you to a hand specialist if the pain is severe.
Aches and pains are part of a normal pregnancy but most can be well managed. If you have any of the symptoms above, and things don’t improve with self-care, check in with your LMC or GP who can then refer you to the right help.
|
OHbaby! fitness expert Renée Vincent is a physiotherapist at Total Mums in Auckland. As a mum of a very busy boy she well knows the physical demands motherhood places on a mama’s body, and loves sharing knowledge to help mamas be at their best. |

AS FEATURED IN ISSUE 46 OF OHbaby! MAGAZINE. CHECK OUT OTHER ARTICLES IN THIS ISSUE BELOW